Abstract

Introduction:
Multiple myeloma is comparatively uncommon cancer, but among blood malignancies it is still the second most common cancer after non-Hodgkin lymphoma. Patients with complications of multiple myeloma (MM) frequently present to the emergency department. There is a lack of data about the health care burden and trends of utilization of emergency department services by MM patients. The objective of this study is to investigate the recent trends in resource utilization in the emergency departments for MM. Furthermore, we aimed to look for the demographic characteristics associated with the subsequent hospitalization of MM patients. We hypothesized that there has been an increase in the utilization of emergency department services for the management of MM patients in recent years. We further hypothesized that subsequent hospitalization rate may be decreasing with the availability of more efficacious and potentially less toxic drugs.
Methods:
For this study we obtained the data from United States National Emergency Department Sample (NEDS) years 2010-2014. For categorical variables, frequencies and proportions were generated and statistical significance was tested using a chi-squared test. Rate of myeloma associated emergency department visits were estimated by using US census population. Patients and hospital characteristics were entered in univariate analysis to predict in-patient admissions from the ED. Multivariable logistic regression was used to predict in-patient admissions for the variables that were found statistically significant in univariate analysis. All tests were two-sided with the statistical significance set at p < 0.05. All analyses were conducted using STATA 14.2v and no missing data was imputed.
Results:
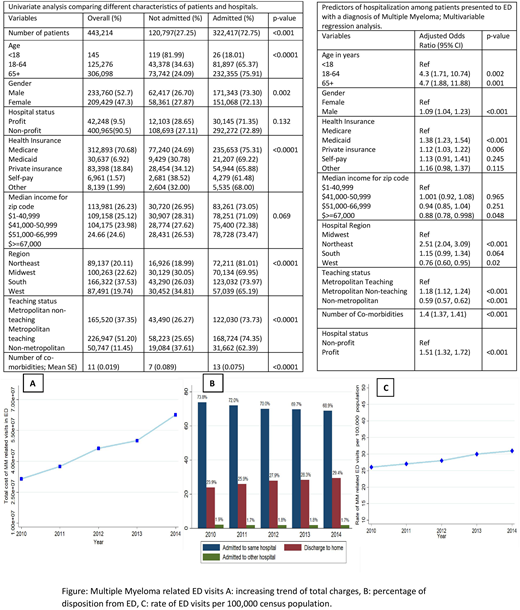
Between 2010 to 2014, approximately 443,214 patients visited emergency departments (ED) with the diagnosis of MM, that accounted for 0.06 % of all emergency department visits. There was an absolute increase of 22% in MM related visits from 80,466 in 2010 to 98,279 in 2014. While the rate of emergency department service utilization by myeloma patient increased significantly by 19% (p=0.04). Overall 73% of myeloma related visits resulted in hospitalization, but over the study period trend of hospitalization decreased. The percentage of patients treated and discharged to home increased from 23% to 29% between 2010 to 2014. Total charges associated with myeloma related visits increased significantly from $315 million to $626 million during 2010 to 2014, with an annual increase in the rate (19.26%: p<0.001). In the multivariable regression analysis several characteristics of patients and hospitals were found to be positively associated with the higher odds of hospitalization following a myeloma related visit. Male gender (OR 1.09, p<0.001), age category 18-64 years (OR 4.3, p=0.002), age of 65 and above (OR 4.7, p=0.001), Medicaid insurance (OR 1.38, p<0.001), northeast location of hospital (OR 2.51, p<0.001), metropolitan non-teaching hospitals (OR 1.18, p<0.001), more number of co-morbidities (OR 1.51, p<0.001) and profit ownership of hospital (OR 1.5, p<0.01).
Conclusion:
Multiple myeloma related emergency department service utilization and total charges are increasing over the observed time limit. While the incidence of hospitalization from emergency department is decreasing overtime. These findings can be explained on the basis of few facts. MM patients are living longer with the availability of newer drugs but remain uncured. Most patients will face relapse after the initial disease control, at which point they may need to utilize ED services more frequently. As better oral or intravenous drugs are available through oncology out-patient offices, limited MM drug choices are available in the hospital, majority of MM patients are discharged sooner from the hospitals resulting in reduced hospital admission rates as well as shorter hospital stay.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal